How Common Is Relapse After Stem Cell Transplant
So, you’re curious about what happens after the confetti settles and the marathon of a stem cell transplant is in the rearview mirror? We’re talking about the long game here, the ‘what-ifs’ and the ‘how-often’ of life post-transplant. Specifically, let’s dive into something that might be a whisper in the back of your mind: relapse. Think of it like this: you’ve just run the most epic marathon of your life, and now you’re wondering about the possibility of needing to lace up those sneakers again. It’s a valid question, and one that deserves a clear, encouraging, and yes, even a touch of a chill answer. Because life after a transplant isn't just about recovery; it's about rebuilding, thriving, and living your best life, even with a few potential hurdles to navigate.
Let’s get straight to it, no beating around the bush. Is relapse after a stem cell transplant a thing? The honest answer is, yes, it is a possibility. However, and this is a big however, it’s not a guarantee, and the likelihood varies wildly depending on a bunch of factors. We’re talking about the type of cancer, the specific transplant you had, and your individual health journey. It’s like trying to predict the weather for next month – we have patterns and probabilities, but no one has a crystal ball.
Think about it like a blockbuster movie. The hero, you, has overcome a massive villain (the disease). The credits are rolling, and we’re all feeling triumphant. But sometimes, in the sequel, a familiar foe might try to make a comeback. The good news? You’re not the same hero who faced that villain the first time. You’ve got a whole new arsenal, a stronger spirit, and a team of experts in your corner. Plus, the makers (your medical team) are constantly innovating, developing new strategies to keep that villain at bay.

So, how common is relapse, really? It’s a number game, and the numbers are getting better and better. For some types of transplants and diseases, the risk can be higher, while for others, it’s significantly lower. For example, in some blood cancers like leukemia or lymphoma that are treated with stem cell transplants, the rate of relapse can range from a few percent to upwards of 30-40% in certain high-risk scenarios. But hold up, don’t let those numbers send you into a tailspin. These are broad figures, and your personal risk is unique.
What’s really encouraging is the progress in this field. Medical science is like that friend who’s always learning new TikTok dances – constantly evolving and improving. We have better ways to assess risk before the transplant, more precise conditioning regimens, and, importantly, more effective strategies for when a relapse does occur. It’s not just about hoping for the best; it’s about having a plan for all the possibilities.
Decoding the Relapse Radar
What influences whether a relapse might happen? It’s a multi-faceted equation, like figuring out the perfect sourdough starter. Several key players are involved:
- The Original Diagnosis: Some cancers are more aggressive or have a higher tendency to return than others. This is a major factor.
- Type of Transplant: Autologous (using your own stem cells) versus allogeneic (using donor stem cells) can have different relapse profiles. Allogeneic transplants often have a lower relapse rate due to the "graft-versus-leukemia" (GvL) or "graft-versus-tumor" (GvT) effect – basically, the donor’s immune system can recognize and attack any lingering cancer cells. It’s like having a built-in security system!
- Disease Status at Transplant: If the disease was more advanced or harder to control before the transplant, there might be a slightly higher risk of recurrence.
- Genetic Factors: Sometimes, the specific genetic mutations within the cancer cells can play a role in their potential to regrow.
- Post-Transplant Monitoring: How closely you’re monitored and how quickly any potential signs of relapse are detected are crucial. Think of it as having super-powered detective skills on your medical team.
It’s important to have open and honest conversations with your hematologist or oncologist about your specific situation. They’re the ultimate guides on this journey, armed with your personal data and a deep understanding of the science. They can give you the most accurate picture of your risk.
The "Graft-Versus-Something" Effect: A Donor’s Secret Weapon
Let’s geek out for a second on the allogeneic transplant. This is where the magic of a donor's immune system really shines. In an allogeneic transplant, the donor’s stem cells, and by extension their immune system, are introduced into your body. This new immune system doesn't just replace your old one; it can also identify foreign (and in this case, diseased) cells that might have survived the conditioning treatment. This is the famed Graft-Versus-Leukemia (GvL) or Graft-Versus-Tumor (GvT) effect. It’s like hiring a highly trained, super-loyal guard dog to patrol your body and sniff out any rogue cells. Pretty neat, right?
This effect is one of the main reasons why allogeneic transplants often have a lower relapse rate compared to autologous transplants for certain diseases. It's a powerful testament to the interconnectedness of our bodies and the incredible capabilities of the immune system. It’s also a reminder of the profound gift a donor provides.
When the Unthinkable Happens: What’s Next?
Okay, so let’s say the unthinkable does happen, and a relapse is detected. It’s natural to feel a wave of emotions – fear, disappointment, maybe even anger. That’s completely valid. But remember, this is not the end of the story. It’s more like a plot twist, a challenging chapter that requires a new strategy.
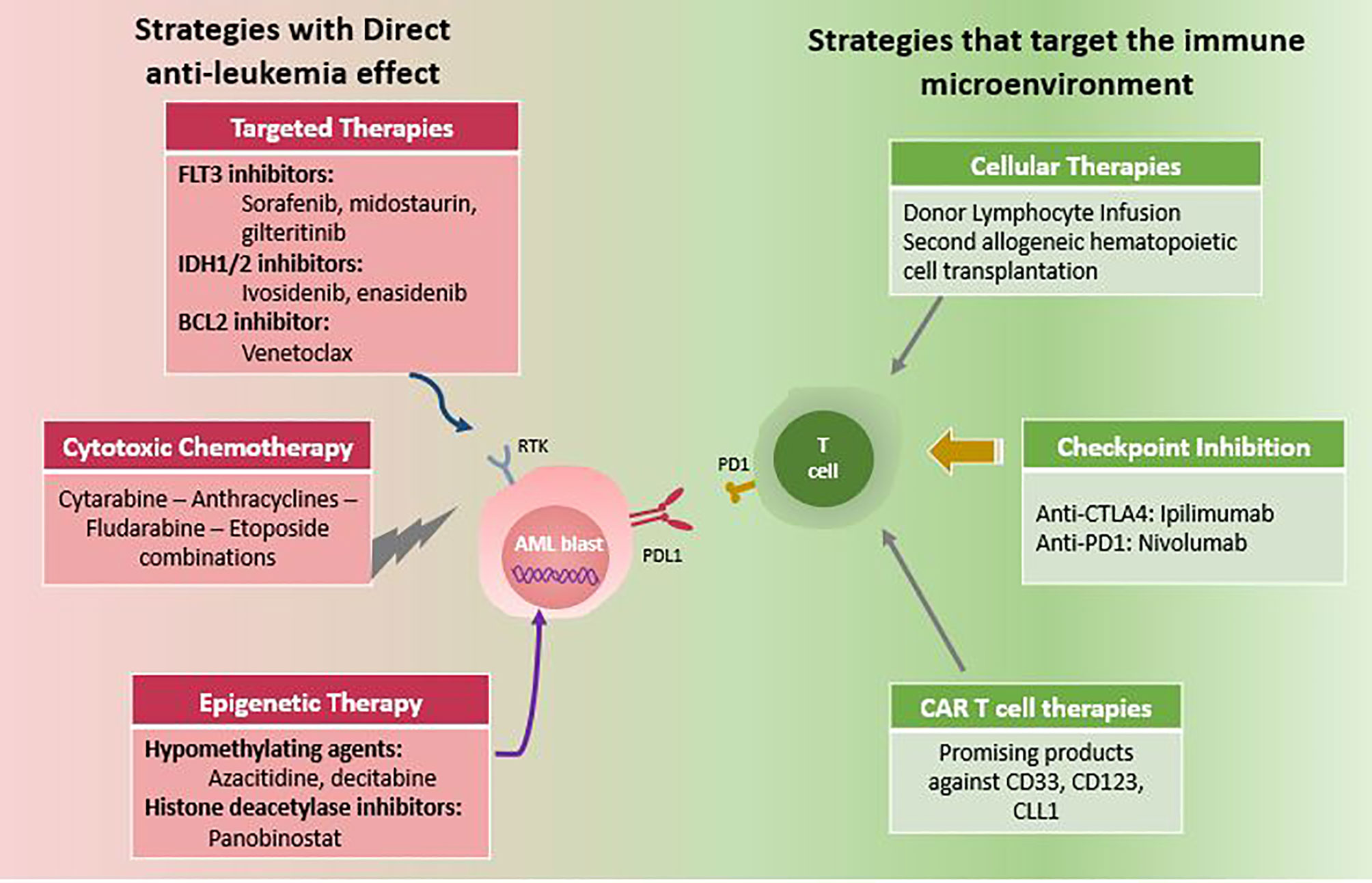
The medical world has made incredible strides in treating relapsed cancers post-transplant. Depending on the type of cancer, the nature of the relapse, and your overall health, there are several options:
- Another Transplant: In some cases, a second stem cell transplant might be an option, either using the same donor or a different one.
- Immunotherapy: This is a hot area of research and treatment, where your own immune system is harnessed and boosted to fight the cancer. Think of it as giving your internal defense system a pep talk and some extra gear.
- Targeted Therapies: These are drugs designed to specifically attack cancer cells by targeting certain genetic mutations or proteins on the cancer cells. It’s like using a laser-guided missile instead of a broad-spectrum bomb.
- Chemotherapy or Radiation: These traditional treatments might still be an option, often in different combinations or dosages.
- Clinical Trials: These are cutting-edge studies that explore new and promising treatments. Participating in a clinical trial can give you access to the latest innovations before they become widely available. It’s like being on the forefront of scientific discovery.
The key here is adaptability and a proactive approach. Your medical team will work tirelessly to find the best course of action for you. It’s a team sport, and you’re the MVP.
Keeping the Odds in Your Favor: Lifestyle Edition
While we can’t control every biological variable, there are definitely things you can do to support your body and potentially reduce the risk of relapse or improve your overall well-being post-transplant. Think of these as your personal wellness power-ups:
- Nutrition is Your Superfood Squad: A balanced, nutrient-rich diet is fundamental. Focus on whole foods, plenty of fruits and vegetables, lean proteins, and healthy fats. Think vibrant colors on your plate – it’s not just pretty, it’s powerful! Consider consulting a registered dietitian who specializes in oncology for personalized advice. They can be your culinary guru.
- Movement is Medicine: Gentle, consistent exercise is incredibly beneficial. It boosts your immune system, improves mood, and helps maintain strength. Start slow and gradually increase intensity as you feel able. Even a brisk walk in the park can make a world of difference. Channel your inner Beyoncé and get those endorphins flowing!
- Sleep Like a Champion: Adequate sleep is crucial for your body’s repair processes. Aim for 7-9 hours of quality sleep per night. Create a relaxing bedtime routine – maybe some chamomile tea and a good book, or a meditation app. Think of sleep as your body’s nightly reset button.
- Stress Management is Your Zen Master: Chronic stress can negatively impact your immune system. Find healthy ways to manage stress, such as mindfulness, meditation, yoga, spending time in nature, or engaging in hobbies you love. Discover your personal calm, whether it’s through a yoga mat or a jam session.
- Stay Connected: Maintaining strong social connections is vital for emotional well-being. Lean on your friends, family, or support groups. Sharing your experiences and connecting with others who understand can be incredibly therapeutic. Think of your support system as your personal cheer squad.
- Hydration Station: Drink plenty of water throughout the day. It helps your body function optimally and aids in flushing out toxins.
- Avoidance is Key: Strictly adhere to any recommended precautions regarding infections. This might include avoiding crowded places or people who are sick, and maintaining good hygiene. It’s about being smart and protecting your hard-won recovery.
- Follow-Up Appointments are Non-Negotiable: This is your VIP pass to staying on top of your health. These appointments are crucial for monitoring your progress, catching any potential issues early, and adjusting your treatment plan as needed. They are your regular check-ins with your health guardian angels.
Remember, these are lifestyle choices that benefit everyone, but they are especially potent tools in the arsenal of someone who has undergone a stem cell transplant. They are about building resilience and nurturing your body’s innate ability to heal and thrive.
Fun Facts and Cultural Nods
Did you know that the concept of replacing diseased cells with healthy ones has been explored for centuries? Ancient Egyptians used blood transfusions, albeit in a very different way, hinting at an early understanding of the body's ability to regenerate. Fast forward to today, and stem cell transplants are a marvel of modern medicine, often likened to a 'reset button' for the immune system.
The dedication and science behind stem cell transplants are truly inspiring. It’s a testament to human ingenuity, much like the creation of the internet or the development of penicillin. And think about it, you’re at the cutting edge of medical history! It's like being part of the "Apollo 13" mission of your own health – overcoming immense challenges with incredible teamwork and innovation.
A Gentle Reflection
Life after a stem cell transplant is a journey of constant learning and adaptation. The question of relapse can linger, but it's important to frame it within the context of immense progress and ongoing care. It's not about dwelling on the 'what if,' but rather about focusing on the 'what is' – living each day with intention, gratitude, and a commitment to your well-being.

Think about it like this: you've just learned a complex new skill, perhaps mastering a musical instrument or learning a new language. There might be moments where you stumble, where you have to revisit a challenging chord or grammar rule. But each time you do, you become stronger, more proficient, and more confident. Relapse, in the rare instances it occurs, is another opportunity to apply what you've learned, to lean on your support systems, and to continue your incredible journey of resilience. It’s a reminder that growth, even after major life events, is always possible, and that your strength is far greater than you might sometimes believe. So, breathe deep, focus on the present, and keep that fabulous life moving forward, one vibrant day at a time.
