How Are Effective Oxygenation And Ventilation Assessed
Ever wonder how doctors know if you're getting enough good air? It's not as simple as looking at you and saying, "Yep, you're breathing fine!" There's a whole secret handshake of tests and gizmos involved. And let's be honest, sometimes the way they assess things feels a little… much. Like they're conducting a symphony of wheezes and gasps, and you're the bewildered orchestra principal.
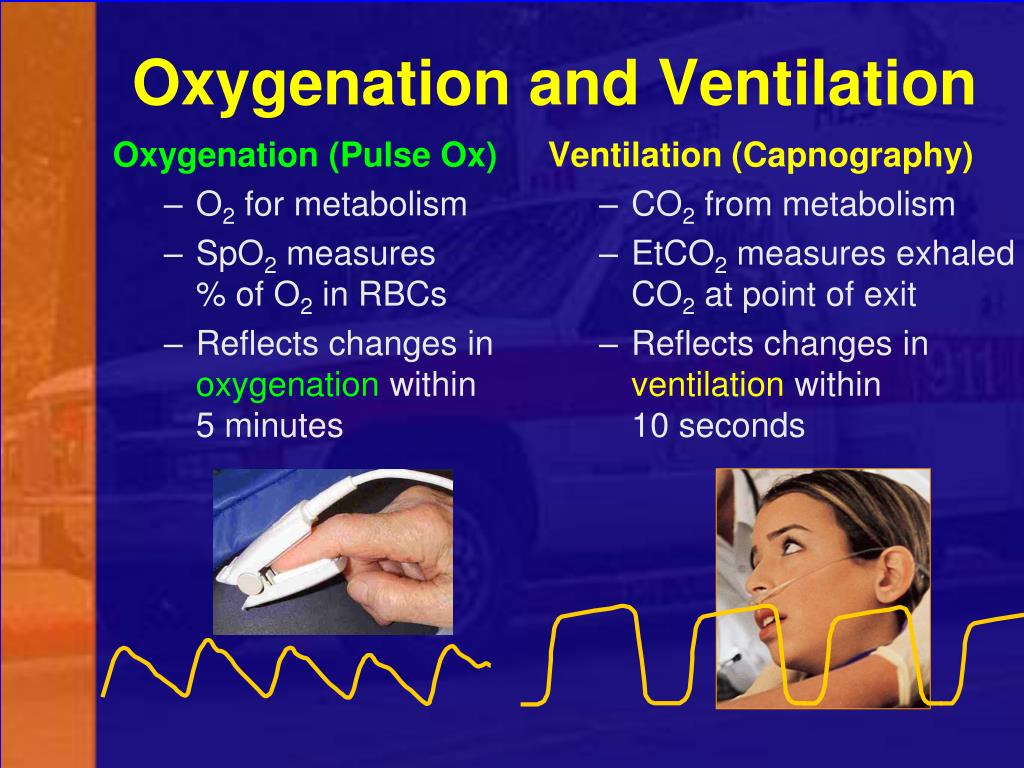
Let's start with the basics: oxygenation. This is all about how much precious oxygen is actually making it into your bloodstream. Think of your red blood cells as tiny delivery trucks, and oxygen is the super important package they’re hauling around. If those trucks aren't loaded up properly, things start to shut down. The most common way to check this, and probably the one you’ve encountered, is the humble pulse oximeter. That little clip they put on your finger? It’s like a miniature detective, shining a light through your skin and blood to figure out how many of those delivery trucks are full. It's pretty neat, really. But sometimes it feels like they're staring at it with bated breath, as if a slight dip means you're about to spontaneously combust. "Oh no, 97%! Quick, inflate a balloon!"
Then there's ventilation. This is the mechanics of it all. It's about getting the air in and out. Are you taking deep, satisfying breaths, or are you doing that shallow, anxious huffing and puffing that makes you feel like you've run a marathon just by thinking about it? Doctors have a few ways to gauge this. They’ll listen to your lungs with their stethoscope. This is the classic. It’s like they’re playing a game of "spot the sound" with your internal organs. They're listening for breath sounds, and whether they're clear and consistent or if there's a suspicious rustle, a whistle, or even a ominous silence where there should be a happy whoosh. Sometimes, you’ll see them tap on your chest too. That's called percussion. It's not a sign of impatience, promise! They're trying to hear how the sound travels through your lungs. Think of it like tapping on a watermelon to see if it's ripe. A hollow sound is good; a dull thud might mean something else is going on.

Now, if things are a bit more complicated, or if the initial checks raise a tiny eyebrow, they might bring out the big guns. One of my personal favorites (and by favorite, I mean the one that makes me feel most like a science experiment) is the arterial blood gas (ABG) test. This involves drawing blood directly from an artery. Yes, an artery. It’s not exactly a spa treatment. They're looking for a much more precise measurement of oxygen and carbon dioxide levels, as well as the pH of your blood. Think of it as a super-duper, high-definition snapshot of what's really happening inside. It tells them not only how much oxygen is getting in, but also how well your body is getting rid of the waste product, carbon dioxide. Too much CO2 and you’re basically holding your breath without even realizing it. Too little, and you might be a bit too enthusiastic with your breathing, which can also cause problems. It’s a delicate balance, much like trying to perfectly toast a piece of bread – too light and it’s disappointing, too dark and it’s a carbonized disaster.
Another way they check ventilation is by looking at your respiratory rate and tidal volume. Respiratory rate is just how many breaths you take per minute. Easy peasy. Tidal volume is a bit fancier. It's the amount of air you inhale and exhale with each normal breath. Sometimes they’ll use a device called a spirometer. This is where you take a big breath and blow into a tube. It's like a fun, albeit slightly undignified, blowing contest. They measure how much air you can move and how fast you can move it. It's all about the power and capacity of your lungs. If your tidal volume is low, it means you’re not moving enough air, even if your rate is normal. It’s like having a small engine in a big car; it’s going to struggle to get you up those hills.
And then, for the real drama, there's the bronchoscopy. Now, this is not your everyday assessment. This involves a tiny camera on a flexible tube being gently (or so they say) inserted into your airways. It's like a miniature submarine exploring the tunnels of your lungs. It allows them to see directly what’s going on inside, looking for blockages, inflammation, or anything that might be interfering with your breathing. While it's incredibly useful, the thought of it alone can make your own breathing feel a little… tight.
The truth is, assessing oxygenation and ventilation is a complex dance. It’s a mix of simple observation, clever technology, and sometimes, a bit of poking and prodding. And while it might seem a bit over the top at times, remember that these are the tools that help keep you breathing easy. So next time a doctor clips that little sensor to your finger, or listens intently to your chest, just give them a knowing smile. They're just doing their best to make sure your internal air conditioning is working perfectly. And hey, at least it's more interesting than watching paint dry, right?
